Role of Hydrogen Inhalation Therapy in Liver Diseases
November 9, 2022 2022-11-28 7:27Role of Hydrogen Inhalation Therapy in Liver Diseases

Role of Hydrogen Inhalation Therapy in Liver Diseases
Table of Contents
Role of Hydrogen Inhalation Therapy in Liver Diseases
Liver is a vital organ inside your body. It aids your body in performing hundreds of tasks, including waste filtering, food digestion, energy storage, and toxin removal. Liver disease implies any medical condition that adversely affects the liver. These conditions may arise from multiple reasons; however they are attributed to liver damage and dysfunction. There are many types of liver diseases and some of these diseases are caused by viruses such as hepatitis. However, other diseases may occur due to excessive consumption of alcohol and drugs (1). Furthermore, long-lasting injury and scarring in liver tissue can lead to cirrhosis. In developed countries, alcoholic liver disease (ALD), hepatitis C virus (HCV), and non-alcoholic steatohepatitis (NASH) are the common causes of cirrhosis. Whereas, in the developing world, hepatitis B virus (HBV) and hepatitis C virus (HCV) are considered the main culprits (2). Globally, liver diseases are responsible for around 2 million deaths per year. Here, 1 million mortalities occur due to complications of cirrhosis, and the other 1 million happen due to hepatitis and hepatocellular carcinoma (HCC) or liver cancer (3). These facts indicate an undeniable burden of liver ailments in the world that need to be minimised by opting advance, cost-effective and wide-range therapeutic strategies.

Currently, many treatment options are available and multiple liver infections and diseases are treated with medications, whereas some severe and end-stage patients may require surgery and liver transplantation. However, alcoholic liver disease, can be managed by reducing or stopping alcohol consumption, lifestyle improvements and losing weight, following a medical course and cautious observation of liver functions (4).
Although, liver transplantation and other advanced treatment options have immensely helped in liver disease management. However, they are associated with many risks and complications, i.e., Ischemia-reperfusion injury (IRI), that can compromise the disease management and a patient’s well-being (5). Therefore, innovative, safe, and effective treatment options should be devised for liver illness treatment, such as molecular hydrogen.
Molecular hydrogen and liver injury
Molecular hydrogen is atomically the smallest gas that can readily diffuse through the body cells. Moreover, it is an inert gas and is present in trace amounts in the atmosphere (6, 7). Hydrogen therapy is gaining immense attention in the clinical setup. It has been reported as an effective treatment strategy for many kinds of diseases (8-11). These therapeutic abilities of molecular hydrogen are attributed to its high affinity, favourable characteristics, and inherent biosafety (12). Hydrogen therapy exerts its beneficial effects via multiple cellular mechanisms featuring its selective anti-inflammatory and antioxidant effects (13-16).
Molecular hydrogen is administered in several ways to treat liver injury. It can be injected as hydrogen-rich saline, drunk as hydrogen-rich water and inhaled as hydrogen gas. Moreover, a bath of hydrogen-rich water and hydrogen-rich eye drops are also used as administration methods. However, the first three methods are frequently opted for the administration of molecular hydrogen in the case of liver ailments (12).
Here, we will learn the therapeutic capacities of hydrogen gas against different liver problems via focusing hydrogen inhalation method. A few hydrogen therapy-treated liver diseases or problems are discussed below:
1. Liver ischemia/reperfusion injury
Hepatic ischemia-reperfusion injury is one f the primary reason for liver transplant failure. It has become an imperative issue due to the rising scenario of liver transplantation regimens in liver diseases.
Hepatic ischemia-reperfusion injury is divided into two distinct categories: warm and cold ischemia-reperfusion injury (IRI). Warm IRI occurs during the surgery when a transient fall in blood flow occurs to the liver. However, cold IRI happens during cold storage of the organ before the transplantation surgery. Both of these IRI types are linked with innate immune responses. Hepatic ischemia-reperfusion injury results in graft dysfunction and increased liver enzymes and biliary structures. Moreover, it increases the risk of acute and chronic transplant rejection and might cause early organ failure in 10% of cases (17). In addition, in some cases, IRI can cause systemic inflammatory response syndrome (SIRS) or multi-organ dysfunction syndrome (MODS) that accounts for high mortality and morbidity rates (18).
Hydrogen inhalation therapy has been extensively used in improving liver ischemia-reperfusion injury. A study evaluated hydrogen inhalation therapy in an experimentally developed hepatic IRI mice model. They observed that inhalation of hydrogen gas at 1-4% concentration reduced liver cell death and decreased the serum levels of liver enzyme and hepatic malondialdehyde. Here, the hepatic malondialdehyde is an indicator or molecular marker of oxidative stress. Hydrogen gas showed a specific hepatoprotective effect and improved ischemia-reperfusion-mediated liver damage by suppressing oxidative stress (19).
Like liver transplantation, liver tissue resection is another surgical procedure in which the damaged part of the liver is removed, and the rest of it regrows. This procedure is also associated with a hepatic ischemia-reperfusion injury that may cause liver failure and can be fatal. Research was carried out in pigs that underwent liver resection surgery. The animals were administered with hydrogen gas during general anaesthesia followed by interoperative preparations and warm ischemia, and reperfusion-induced liver injury. The liver tissue sections from IRI and non-IRI halves of the liver were then analyzed to evaluate the effects of inhaled hydrogen compared to the control (with no administration of hydrogen gas). The results showed that hydrogen gas undeniably suppressed the ischemia-reperfusion damage-related levels of oxidative stress. Thus the study suggests that hydrogen inhalation can exert protective effects against ischemia-reperfusion liver damage during tissue resection surgery (20).
Another similar study was performed to evaluate the protective effect of molecular hydrogen gas in experimentally developed ischemia-reperfusion liver injury porcine models. The investigations revealed that the hydrogen gas showed a remarkable protective effect against ischemia-reperfusion injury in liver. Moreover, it was found safe and effective against the problem. All these attributes recommend molecular hydrogen use in clinical settings (21).
Additionally, a study was conducted to examine the protective effect of hydrogen inhalation in pigs which underwent massive hepatectomy. Herein, hydrogen inhalation significantly attenuated the ischemia-reperfusion liver injury by decreasing oxidative stress and inflammation. These positive effects of hydrogen gas suggest it as a potential treatment in the clinic (22).
Researchers have also investigated the mechanisms through which hydrogen gas exerts protective effects against ischemia-reperfusion liver injury. A similar study investigated the effect of hydrogen inhalation in a liver IRI animal model. The results indicated that administration of 2% hydrogen gas for 1 hour remarkably lessened the serum levels of liver enzymes, i.e., alanine aminotransferase (ALT) and aspartate aminotransferase (AST). Alongside, the treatment reduced morphological damage and the expression of cytokines involving TNF-α, IL-6, IL-1β and Egr-1 (early growth response protein 1). Further, the analysis showed that hydrogen treatment before organ transplantation protected against hepatic IRI via stimulation of the NF-κB signaling pathway (23).
Likewise, research was carried out in an ischemia-reperfusion liver injury mice model. In this study, the mice models received high hydrogen gas concentrations immediately after the surgery. After 6h of IRI induction, different experiments were conducted to evaluate the hydrogen gas effect and its mechanism of action. The results showed that high hydrogen gas concentrations effectively ameliorated liver function, suppressed serum levels of inflammatory cytokines, and impeded the death of the liver cell. Moreover, the detailed study found that hydrogen mediates these cellular functions via activation of the PI3K/AKT signalling pathway (24).
2. Alcoholic liver disease
Alcohol-induced liver injury covers a spectrum of disorders. It occurs due to excessive consumption of alcohol. Alcoholic liver disease begins with the accumulation of fat in liver cells that develop a fatty liver, also called steatosis. Afterwards, fatty liver gradually progress to alcoholic hepatitis stage that is attributed by inflammation of liver cells and ultimately culminate at cirrhosis which is the irreversible and most advanced stage of liver damage (25).
Alcoholic liver disease pathogenesis features oxidative stress, alteration of liver metabolism, genetic susceptibility, cytokine and chemokines mediated inflammation, modifications in liver regenerative process and change in immunity etc. (26-29). Hydrogen gas is reported to play an imperative part in controlling hepatic redox, inflammatory, and immune homeostasis. There is limited elaboration of hydrogen therapy in alcoholic liver disease management. However, a recent study used hydrogen gas therapy for alcohol-induced liver injury mice model. In this study, hydrogen gas administration alleviated alcohol-induced liver damage by attenuating the activation of the JNK signalling. Moreover, the therapy resulted in the decrease of serum levels of AST and ALT enzymes that were upsurged by alcohol induce liver injury. These enzyme levels are measured to monitor liver functioning (30).
3. Non-alcoholic fatty liver disease
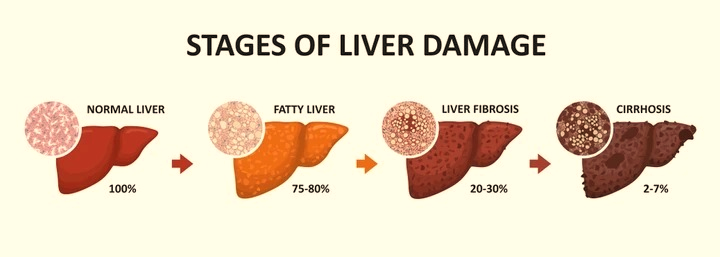
Non-alcoholic fatty liver disease (NAFLD) is the leading cause of severe liver damage (cirrhosis) and liver cancer (hepatocellular carcinoma), with a global prevalence of 25%. In NAFLD, liver damage sets off with the accumulation of fats (steatosis stage) with or without slight inflammation, known as non-alcoholic fatty liver. Later this condition turns to non-alcoholic steatohepatitis or NASH which is attributed by accelerated fibrosis development and necroinflammation compared to the earlier non-alcoholic fatty liver stage. NAFLD prevention and treatment are crucially associated to weight reduction and a healthy lifestyle (31). However, due to the complex pathophysiology and extensive heterogeneity of non-alcoholic fatty liver disease phenotypes, a proactive treatment approach is required, such as molecular hydrogen gas therapy.
Many research studies have examined the effectiveness of hydrogen gas against non-alcoholic fatty liver disease. One such study was designed via inducing the hepatocyte steatosis through carbon tetrachloride (CCl4) chemical. It is a widely used method to experimentally induce liver injury in in vivo experiments. This study exhibited that hydrogen gas inhalation in rat models significantly reduced steatosis in liver cells and increased uncoupling protein 2. Detailed analysis suggested that hydrogen gas might exert its protective role in liver cells via suppressing intracellular reactive oxygen species, upregulating the expression of the uncoupling protein 2 and affecting lipid metabolism in hepatic cells (32).
Furthermore, hydrogen inhalation therapy effects were studied in a rat model of metabolic syndrome with non-alcoholic fatty liver disease. In this study, the rat disease models inhaled hydrogen gas at low and high concentrations for ten weeks. After the experiment, the analysis of the results showed that hydrogen is protective against the liver injury. It positively influences the general state of the liver along with its histology, liver function indicators and lipid metabolism parameters to alleviate the non-alcoholic fatty liver condition in metabolic syndrome rat models (33).
A randomized clinical trial of hydrogen inhalation was performed to study its effect on non-alcoholic fatty liver disease subjects. The trial was carried out for 13 weeks in 43 subjects. After the completion of the trial, significant improvement in liver enzymes and serum levels of lipid content was observed. Moreover, the study revealed that hydrogen gas inhalation alleviates non-alcoholic fatty liver disease in moderate to severe patients. Additionally, the protective role of hydrogen was attributed to its ability to activate autophagy in liver cells (34).
4. Sepsis-induced liver injury
Sepsis is the body’s extreme response to an infection. It induced intense changes in the ability of liver to transport bilirubin and bile acids to the hepatic canaliculi, thereby resulting in cholestasis. It is a condition in which bile release from the liver is impeded. Sepsis-linked hepatic dysfunction can be categorized into jaundice and hypoxic hepatitis. Jaundice is a more frequent condition in the context of sepsis (35). Hydrogen inhalation therapy has been utilized to ameliorate this condition via regulation of cellular mechanisms.
A recent study showed the protective effect of hydrogen gas in mice models of sepsis-induced liver injury. Hydrogen gas improved liver damage by the regulation of mitophagy. Mitophagy is a type of autophagy that is crucial to sepsis mediated organ damage. It is basically the removal of damaged mitochondria that aid in maintaining proper cellular functions. Further extensive research showed that 2% hydrogen gas inhalation therapy exhibited protective effects via mitochondrial outer-membrane protein FUNDC1-mediated mitophagy (36).
All these profound studies provide insights into the use of molecular hydrogen gas in liver diseases and suggest a safe and effective treatment approach. However, the available studies are limited to favour its clinical use. Therefore, more detailed animal-based liver disease model studies are required against different liver problems to bring the therapy to the clinical settings.
Reference
- Dolganiuc A. Alcohol and viral hepatitis: role of lipid rafts. Alcohol research: current reviews. 2015;37(2):299.
- Naveau S, Perlemuter G, Balian A. [Epidemiology and natural history of cirrhosis]. La Revue du praticien. 2005;55(14):1527-32.
- Mokdad AA, Lopez AD, Shahraz S, Lozano R, Mokdad AH, Stanaway J, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC medicine. 2014;12(1):1-24.
- Marsano LS, Mendez C, Hill D, Barve S, McClain CJ. Diagnosis and treatment of alcoholic liver disease and its complications. Alcohol research & health. 2003;27(3):247.
- Zhai Y, Petrowsky H, Hong JC, Busuttil RW, Kupiec-Weglinski JW. Ischaemia–reperfusion injury in liver transplantation—from bench to bedside. Nature reviews Gastroenterology & hepatology. 2013;10(2):79-89.
- Saitoh Y, Okayasu H, Xiao L, Harata Y, Miwa N. Neutral pH hydrogen-enriched electrolyzed water achieves tumor-preferential clonal growth inhibition over normal cells and tumor invasion inhibition concurrently with intracellular oxidant repression. Oncology Research Featuring Preclinical and Clinical Cancer Therapeutics. 2008;17(6):247-55.
- Lafay V, Barthelemy P, Comet B, Frances Y, Jammes Y. ECG changes during the experimental human dive HYDRA 10 (71 atm/7,200 kPa). Undersea & hyperbaric medicine: journal of the Undersea and Hyperbaric Medical Society, Inc. 1995;22(1):51-60.
- Hashimoto M, Katakura M, Nabika T, Tanabe Y, Hossain S, Tsuchikura S, et al. Effects of hydrogen-rich water on abnormalities in a SHR. Cg-Lepr cp/NDmcr rat-a metabolic syndrome rat model. Medical Gas Research. 2011;1(1):1-6.
- Kajiyama S, Hasegawa G, Asano M, Hosoda H, Fukui M, Nakamura N, et al. Supplementation of hydrogen-rich water improves lipid and glucose metabolism in patients with type 2 diabetes or impaired glucose tolerance. Nutrition Research. 2008;28(3):137-43.
- Ito M, Ibi T, Sahashi K, Ichihara M, Ito M, Ohno K. Open-label trial and randomized, double-blind, placebo-controlled, crossover trial of hydrogen-enriched water for mitochondrial and inflammatory myopathies. Medical gas research. 2011;1(1):1-8.
- Matsumoto S, Ueda T, Kakizaki H. Effect of supplementation with hydrogen-rich water in patients with interstitial cystitis/painful bladder syndrome. Urology. 2013;81(2):226-30.
- Shi J, Duncan B, Kuang X. Hydrogen treatment: a novel option in liver diseases. Clinical Medicine. 2021;21(2):e223.
- Yoon KS, Huang XZ, Yoon YS, Kim S-K, Song SB, Chang BS, et al. Histological study on the effect of electrolyzed reduced water-bathing on UVB radiation-induced skin injury in hairless mice. Biological and Pharmaceutical Bulletin. 2011;34(11):1671-7.
- Nakayama M, Nakano H, Hamada H, Itami N, Nakazawa R, Ito S. A novel bioactive haemodialysis system using dissolved dihydrogen (H2) produced by water electrolysis: a clinical trial. Nephrology Dialysis Transplantation. 2010;25(9):3026-33.
- Yanagihara T, Arai K, Miyamae K, Sato B, Shudo T, Yamada M, et al. Electrolyzed hydrogen-saturated water for drinking use elicits an antioxidative effect: a feeding test with rats. Bioscience, biotechnology, and biochemistry. 2005;69(10):1985-7.
- Chen Y, Jiang J, Miao H, Chen X, Sun X, Li Y. Hydrogen-rich saline attenuates vascular smooth muscle cell proliferation and neointimal hyperplasia by inhibiting reactive oxygen species production and inactivating the Ras-ERK1/2-MEK1/2 and Akt pathways. International Journal of Molecular Medicine. 2013;31(3):597-606.
- Rampes S, Ma D. Hepatic ischemia-reperfusion injury in liver transplant setting: Mechanisms and protective strategies. Journal of Biomedical Research. 2019;33(4):221.
- Guo WA. The search for a magic bullet to fight multiple organ failure secondary to ischemia/reperfusion injury and abdominal compartment syndrome. The Journal of Surgical Research. 2012;184(2):792-3.
- Fukuda K-i, Asoh S, Ishikawa M, Yamamoto Y, Ohsawa I, Ohta S. Inhalation of hydrogen gas suppresses hepatic injury caused by ischemia/reperfusion through reducing oxidative stress. Biochemical and Biophysical Research Communications. 2007;361(3):670-4.
- Malý O, Zajak J, Hyšpler R, Turek Z, Astapenko D, Jun D, et al. Inhalation of molecular hydrogen prevents ischemia-reperfusion liver damage during major liver resection. Annals of Translational Medicine. 2019;7(23).
- Matsuno N, Watanabe R, Kimura M, Iwata S, Fujiyama M, Kono S, et al., editors. Beneficial effects of hydrogen gas on porcine liver reperfusion injury with use of total vascular exclusion and active venous bypass. Transplantation Proceedings; 2014: Elsevier.
- Xiang L, Tan J-W, Huang L-J, Jia L, Liu Y-Q, Zhao Y-Q, et al. Inhalation of hydrogen gas reduces liver injury during major hepatotectomy in swine. World journal of gastroenterology: WJG. 2012;18(37):5197.
- Zhang C-B, Tang Y-C, Xu X-J, Guo S-X, Wang H-Z. Hydrogen gas inhalation protects against liver ischemia/reperfusion injury by activating the NF-κB signaling pathway. Exp Ther Med. 2015;9(6):2114-20.
- Li H, Chen O, Ye Z, Zhang R, Hu H, Zhang N, et al. Inhalation of high concentrations of hydrogen ameliorates liver ischemia/reperfusion injury through A2A receptor mediated PI3K-Akt pathway. Biochemical pharmacology. 2017;130:83-92.
- Patel R, Mueller M, Doerr C. Alcoholic liver disease (nursing). 2021.
- Seitz HK, Bataller R, Cortez-Pinto H, Gao B, Gual A, Lackner C, et al. Alcoholic liver disease. Nature reviews Disease primers. 2018;4(1):1-22.
- Gao B, Bataller R. Alcoholic liver disease: pathogenesis and new therapeutic targets. Gastroenterology. 2011;141(5):1572-85.
- Louvet A, Mathurin P. Alcoholic liver disease: mechanisms of injury and targeted treatment. Nature reviews Gastroenterology & hepatology. 2015;12(4):231-42.
- Bajaj JS. Alcohol, liver disease and the gut microbiota. Nature Reviews Gastroenterology & Hepatology. 2019;16(4):235-46.
- Zhang Y, Bi M, Chen Z, Dai M, Zhou G, Hu Y, et al. Hydrogen gas alleviates acute alcohol‑induced liver injury by inhibiting JNK activation. Experimental and therapeutic medicine. 2021;21(5):1-7.
- Powell EE, Wong VW, Rinella M. Non-alcoholic fatty liver disease. Lancet (London, England). 2021;397(10290):2212-24.
- Wang J, Cheng Q, Fang J, Ding H, Liu H, Fang X, et al. A Preliminary Study on the Effect of Hydrogen Gas on Alleviating Early CCl4-Induced Chronic Liver Injury in Rats. Antioxidants. 2021;10(12):1933.
- Liu B, Xue J, Zhang M, Wang M, Ma T, Zhao M, et al. Hydrogen inhalation alleviates nonalcoholic fatty liver disease in metabolic syndrome rats. Molecular medicine reports. 2020;22(4):2860-8.
- Tao G, Zhang G, Chen W, Yang C, Xue Y, Song G, et al. A randomized, placebo‐controlled clinical trial of hydrogen/oxygen inhalation for non‐alcoholic fatty liver disease. Journal of Cellular and Molecular Medicine. 2022;26(14):4113-23.
- Wang D, Yin Y, Yao Y. Advances in sepsis-associated liver dysfunction. Burns & Trauma. 2014;2(3):2321-3868.132689.
- Yan M, Yu Y, Mao X, Feng J, Wang Y, Chen H, et al. Hydrogen gas inhalation attenuates sepsis-induced liver injury in a FUNDC1-dependent manner. International Immunopharmacology. 2019;71:61-7.



